Prevalence of Potentially Inappropriate Medication Use in Older Drivers: AAA LongROAD Study
This research brief asses the use of potentially inappropriate medications (PIMs) in older adults that is associated with high levels morbidity, mortality and health care expenditures.
November 2018
Suggested Citation
For media inquiries, contact:
Tamra Johnson
202-942-2079
TRJohnson@national.aaa.com
Abstract
Introduction
Use of potentially inappropriate medications (PIMs) in older adults is associated with high levels of morbidity, mortality and health care expenditures. The Beers Criteria are a widely used tool for identifying PIMs that should generally be avoided in older adults. The American Geriatrics Society 2015 Beers Criteria were applied to baseline data collected from a “brown-bag” review of medications for the Longitudinal Research on Aging Drivers (LongROAD) participants to examine the prevalence and correlates of PIM use. Overall, 18.5% of the study sample used at least one PIM. The most commonly used therapeutic category of PIM was benzodiazepines (accounting for 16.6% of the total PIMs identified), followed by nonbenzodiazepine hypnotics (15.2%), antidepressants (15.2%) and first-generation antihistamines (10.5%). The variable most predictive of PIM use was the total number of medications being taken. Other factors associated with a significantly increased use of PIMs were being female, being white and living in an urban residence. Use of PIMs is fairly common in older drivers and often involves medications known to impair driving ability and increase crash risk. In order to improve traffic safety among older drivers, drivers should be aware of the types of medications they are taking to ensure optimal safety behind the wheel.
Key Findings
- 545 out of the 2,949 study participants with medication data used at least one PIM that should generally be avoided, yielding a point prevalence of 18.5%.
- The odds of PIM use increase with the number of medications taken and are particularly high among white, female older drivers in urban areas.
- The PIMS most commonly used by older drivers are benzodiazepines, nonbenzodiazepine hypnotics, antidepressants and first-generation antihistamines, all of which have been linked to driving impairment and increased crash risk.
Methodology
Information presented in this documented used data from the LongROAD project – a multisite prospective cohort study of 2,990 active drivers ages 65-79 years old, from primary care clinics or health care systems in five study sites (Ann Arbor, Michigan; Baltimore, Maryland; Cooperstown, New York; Denver, Colorado; and San Diego, California). Following informed consent, each driver was assessed at baseline with standardized research protocols and instruments, which included functional performance tests, a questionnaire interview and a brown-bag review of medications, in which research staff instructed the study participants to bring all current medications (both prescribed and over-the-counter) and supplements. Medication data collected at baseline were coded according to the pharmacologic/therapeutic classification system established by the American Society of Health-System Pharmacists in the American Hospital Formulary Service (AHFS) Clinical Drug Information. The AHFS classification system groups medications with similar pharmacologic, therapeutic and chemical characteristics in a four-tier hierarchy. Noncoded medications included foodlike items (e.g. spices or protein), homeopathic products and other supplements. The 2015 American Geriatrics Society (AGS) Beers Criteria for PIM use in older adults were applied to the AHFS-coded medication data to identify PIMs in the study sample. Prevalence of PIM use was calculated according to demographic characteristics and analyzed in relation to the residence locations of LongROAD participants.
Results
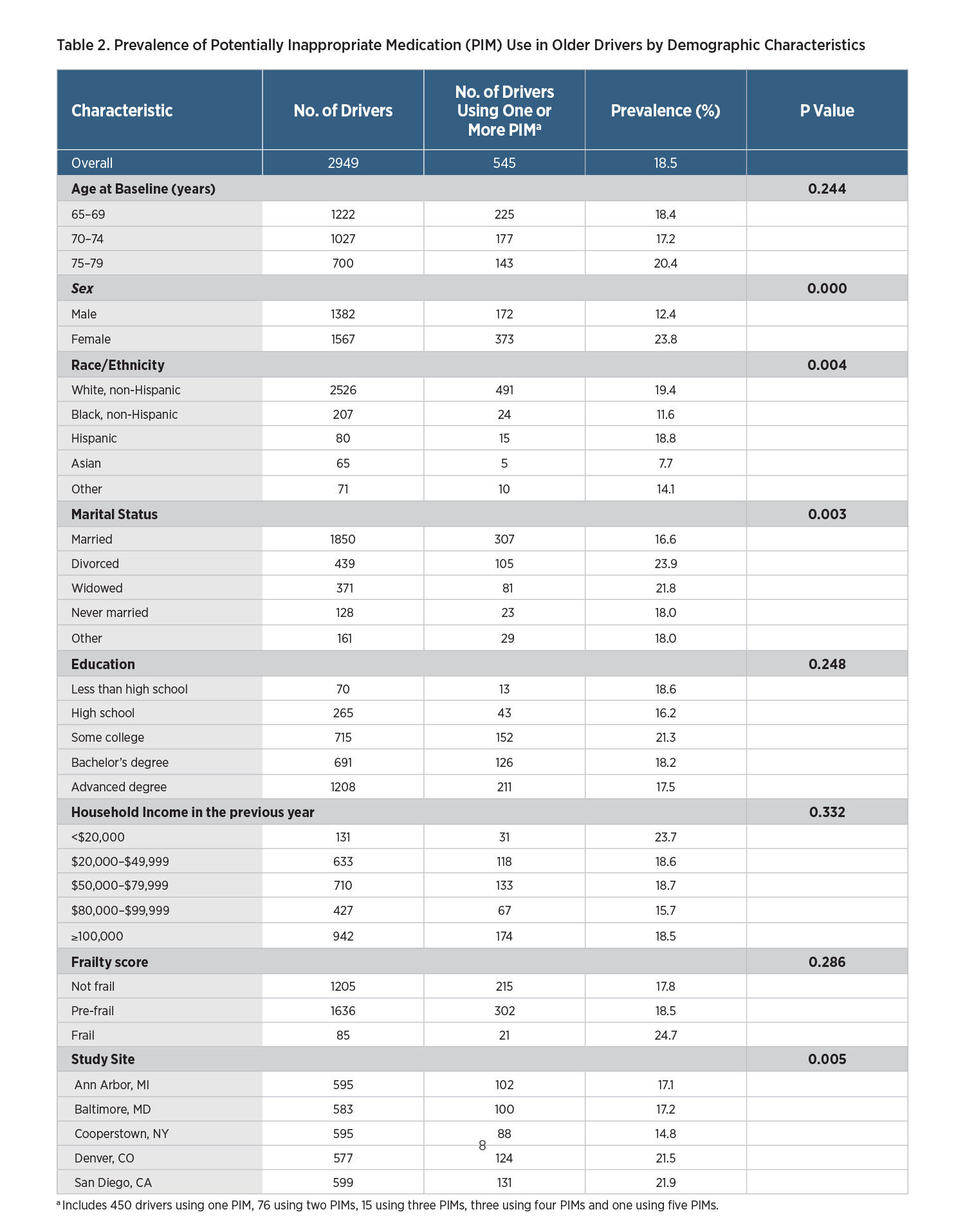
Overall, 545 out of the 2,949 study participants with medication data available used at least one PIM that should generally be avoided, yielding a point prevalence of 18.5%. The prevalence of PIM use varied significantly with age, sex, race/ethnicity and marital status (Table 1). Specifically, higher prevalence of PIM use was found in drivers who were 75-79 years of age, female, white or not currently married (Table 1). The most pronounced difference in the prevalence of PIM use with regard to demographic characteristics was between sexes, with female drivers being nearly twice as likely as male drivers to use PIMs (23.8% vs. 12.4%, p<0.0001). When measured by frailty score, the health status of the study participants was mostly good, with 41.2% being classified as not frail, 55.9% as prefrail, and 2.9% as frail. Additionally, the prevalence of PIM use varied with study sites, ranging from 14.8% for drivers recruited in Cooperstown, New York, to 21.9% for drivers recruited in San Diego, California (Table 1). In terms of urbanicity, the prevalence of PIM use among older drivers in urban areas was 20.1%, significantly higher than in suburban areas (13.6%) and rural areas (14.7%).
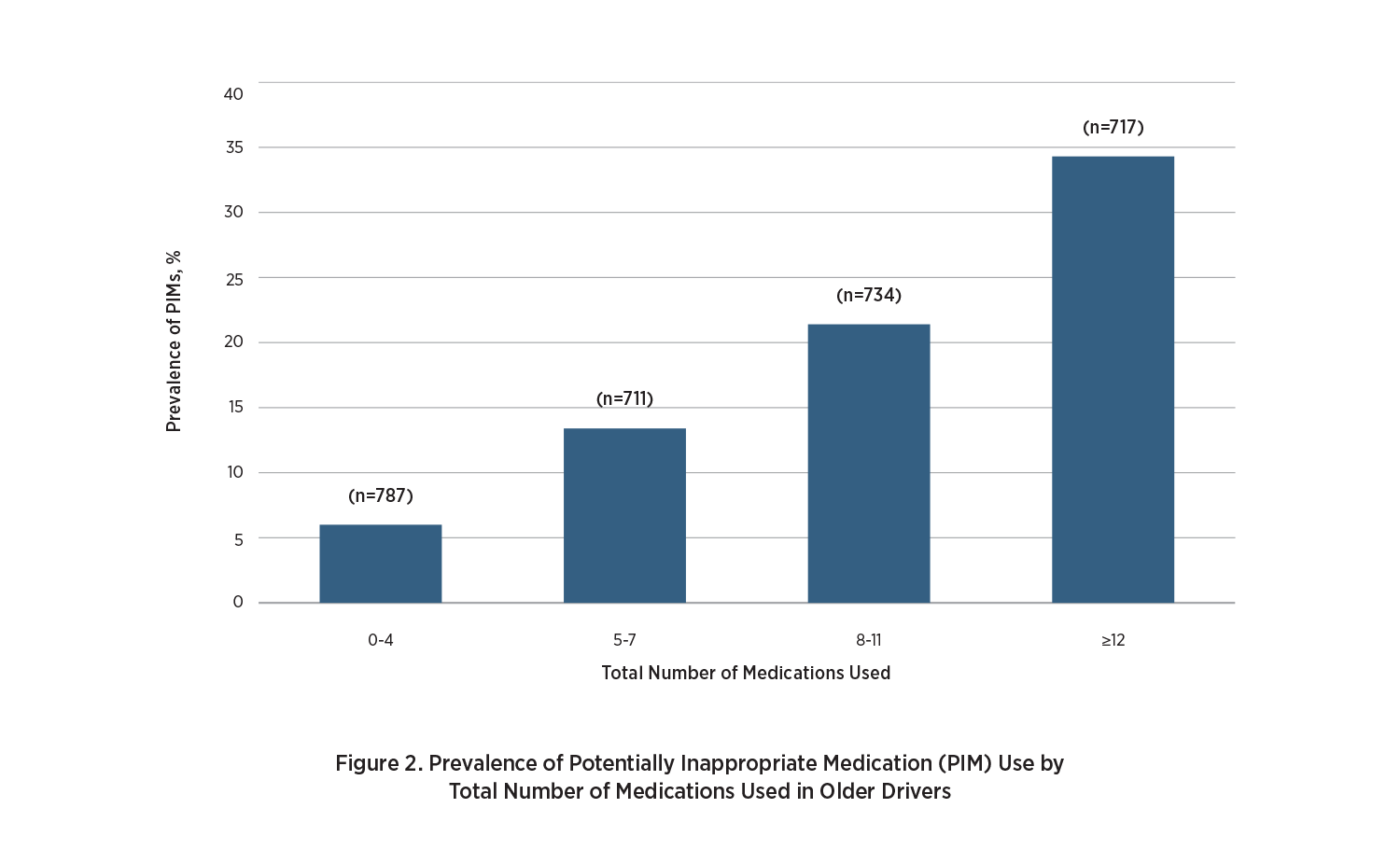
Furthermore, the prevalence of PIM use increased progressively with the number of medications used. Over one-third (34.3%) of older drivers who were on 12 or more medications used PIMs, compared with 6.0% of those on four or fewer medications, 13.4% of those on five to seven medications and 21.4% of those on eight to 11 medications. Drivers who were female, white or living in urban areas showed significantly increased risk of PIM use. The use of multiple PIMs was common among older drivers. Of the 545 PIM users, 95 (17.4%) used two or more PIMs. The most frequently used therapeutic category of PIM was benzodiazepines (e.g., Diazepam or Valium typically used to treat anxiety, insomnia and seizures, and to relax the muscles), accounting for 16.6% of the total PIMs identified.
Suggested Citation
For media inquiries, contact:
Tamra Johnson
202-942-2079
TRJohnson@national.aaa.com